WITH BATED BREATHIt will probably take five years until such a product is on the market, but doctors who know about a new technology for noninvasive measurement of the breathing of surgery patients, adults with sleep apnea and babies at risk of sudden infant death syndrome (SIDS) are looking forward to it.University of Utah engineers involved with the invention previously built wireless networks that can see through walls. Because the technique uses off-the-shelf wireless transceivers similar to those used in home computer networks, “the cost of this system will be cheaper than existing methods of monitoring breathing,” says electrical engineering Prof. Neal Patwari, the senior author of the study of the new method. He says a network of wireless transceivers around a bed can measure breathing rates and alert someone if breathing stops, without the need for any tubes or wires to be connected to the patient.“We can use this to increase the safety of people who are under sedation after surgery by knowing if they stop breathing,” he says. “We also envision a product that parents put around their baby’s crib to alert them if the baby stops breathing. It might be useful for babies at risk of SIDS.”The American Academy of Pediatrics (AAP), whose longtime policy against the use of breathing monitors at home has been endorsed by their Israeli counterparts, says there is no evidence that such monitors are effective for preventing SIDS. Since 2005, the group has opposed the use of breathing monitors to prevent SIDS, but has said they “may be useful in some infants who have had an apparent life-threatening event,” including some combination of apnea (abnormal interruptions in breathing), color change, limpness and choking or gagging.Some opposition to SIDS monitors is based on fears parents will depend on monitors instead of following other, more effective medical measures, including always placing babies on their backs to sleep, keeping redundant bedding and soft objects out of the crib, and not having babies share a bed with adults. But many parents feel safer with the devices and are willing to spend money on them.“The AAP recognizes that monitors may be helpful to allow rapid recognition of apnea, airway obstruction, respiratory failure, interruption of supplemental oxygen supply, or failure of mechanical respiratory support,” the group stated recently.In addition to other possible uses, Patwari wants to conduct research with doctors to test his method as an infant-breathing monitor, and, if it proves useful, develop it as a medical device that would need US federal government approval. He also says it may be useful for adults with sleep apnea, which causes daytime fatigue and impairs a person’s performance.SIDS monitors now on the market include FDAapproved medical devices that measure heart rate and respiration and are connected to babies with wires, electrodes and/or belts. Other monitors, which are non-medical and over-the-counter versions, detect a lack of sound or use mattress sensors to detect a lack of movement. To decide if someone is breathing or not, the University of Utah’s wireless system uses a computer algorithm – basically, a set of formulas. A number larger than 1.5 indicates breathing has been detected.
New Worlds: Bacterial toxins; Breathing of surgery patients
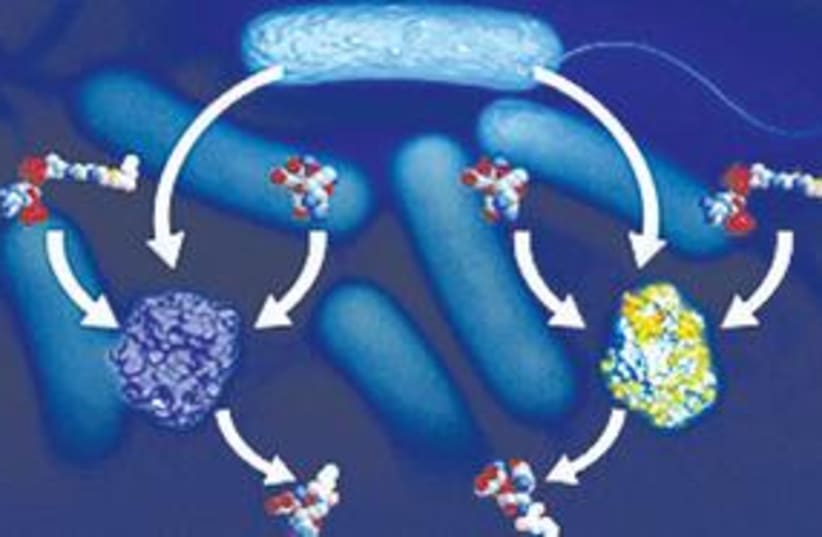
Hebrew University of Jerusalem researchers have discovered a path to blocking bacterial toxins that until now have resisted all conventional treatments.
WITH BATED BREATHIt will probably take five years until such a product is on the market, but doctors who know about a new technology for noninvasive measurement of the breathing of surgery patients, adults with sleep apnea and babies at risk of sudden infant death syndrome (SIDS) are looking forward to it.University of Utah engineers involved with the invention previously built wireless networks that can see through walls. Because the technique uses off-the-shelf wireless transceivers similar to those used in home computer networks, “the cost of this system will be cheaper than existing methods of monitoring breathing,” says electrical engineering Prof. Neal Patwari, the senior author of the study of the new method. He says a network of wireless transceivers around a bed can measure breathing rates and alert someone if breathing stops, without the need for any tubes or wires to be connected to the patient.“We can use this to increase the safety of people who are under sedation after surgery by knowing if they stop breathing,” he says. “We also envision a product that parents put around their baby’s crib to alert them if the baby stops breathing. It might be useful for babies at risk of SIDS.”The American Academy of Pediatrics (AAP), whose longtime policy against the use of breathing monitors at home has been endorsed by their Israeli counterparts, says there is no evidence that such monitors are effective for preventing SIDS. Since 2005, the group has opposed the use of breathing monitors to prevent SIDS, but has said they “may be useful in some infants who have had an apparent life-threatening event,” including some combination of apnea (abnormal interruptions in breathing), color change, limpness and choking or gagging.Some opposition to SIDS monitors is based on fears parents will depend on monitors instead of following other, more effective medical measures, including always placing babies on their backs to sleep, keeping redundant bedding and soft objects out of the crib, and not having babies share a bed with adults. But many parents feel safer with the devices and are willing to spend money on them.“The AAP recognizes that monitors may be helpful to allow rapid recognition of apnea, airway obstruction, respiratory failure, interruption of supplemental oxygen supply, or failure of mechanical respiratory support,” the group stated recently.In addition to other possible uses, Patwari wants to conduct research with doctors to test his method as an infant-breathing monitor, and, if it proves useful, develop it as a medical device that would need US federal government approval. He also says it may be useful for adults with sleep apnea, which causes daytime fatigue and impairs a person’s performance.SIDS monitors now on the market include FDAapproved medical devices that measure heart rate and respiration and are connected to babies with wires, electrodes and/or belts. Other monitors, which are non-medical and over-the-counter versions, detect a lack of sound or use mattress sensors to detect a lack of movement. To decide if someone is breathing or not, the University of Utah’s wireless system uses a computer algorithm – basically, a set of formulas. A number larger than 1.5 indicates breathing has been detected.