A light from Ethiopia
Volunteer medical work gives doctor-to-be the perspective he seeks to crystallize the course of his life.
Breakfast, lunch and dinner. A clean shave and a hot shower. Three pillows, soft sheets and a down comforter. Electricity. Running water. An entire room designated for purging waste from our bodies with the usual necessities and amenities, such as water, toilet paper, soap and towels.
When I stepped into Ethiopia for the first time on September 26, these seeming necessities would all but vanish for the next 12 days.
The only people I know who had confronted anything like this reality are from my grandparents' generation - Holocaust survivors, like my grandmother. My kind of "crisis" was the flight we missed on our way to Ethiopia because I forgot to move my clock an hour forward after leaving Israel.
My first 18 years were carefully crafted by my parents and the past seven, albeit slightly more bumpy, were mostly the same, except my parents participated as experienced coaches. From consecrations and bar mitzvas to private school education and school trips to family vacations and spring breaks, I consider myself very fortunate to live a privileged life. However, with this more than comfortable lifestyle as I finish medical school in Tel Aviv, my desire to do something outside the box finally rose to a boil.
Initially apprehensive, my mind swirled with uncertainties. Would I like the people I am going with? How would I keep in touch with my fiancée? What would I eat on a regular basis? Where would we be sleeping? What about all the disease? HIV? Yellow fever? Malaria? Only my determination to do something outside my comfort zone, beyond the world that is familiar to me, drove me forward.
We landed in Addis Ababa on an overcast afternoon. But our welcome was overwhelmingly beautiful.
When most of us travel and leave the airport, we see the men huddling around the automatic doors, cellphone in one hand, Bluetooth in one ear and a sign - sometimes computer typed and sometimes written with a black Sharpie - bearing someone's last name. We look, curiously, wondering if we will see our own family name, knowing, though, that the driver is waiting for someone else.
Here, by contrast, were greeted by three smiling children with three different colored roses, one for each of us, and four other representatives, all equally excited to meet us, from the orphanage where would be spending the next three days.
WE DROVE to the Tsige Tadese orphanage, about 25 kilometers from the capital in a rural part of the country. As this was my first foray into the developing world, I was in immediate culture shock. The streets were alive with people. It was different, though. People were not buying music, T-shirts and whatever else you can think of at an open market. Rather, they were buying staples, such as flour, water and toilet paper. The roads were littered with potholes and we swerved left and right to avoid a blown tire.
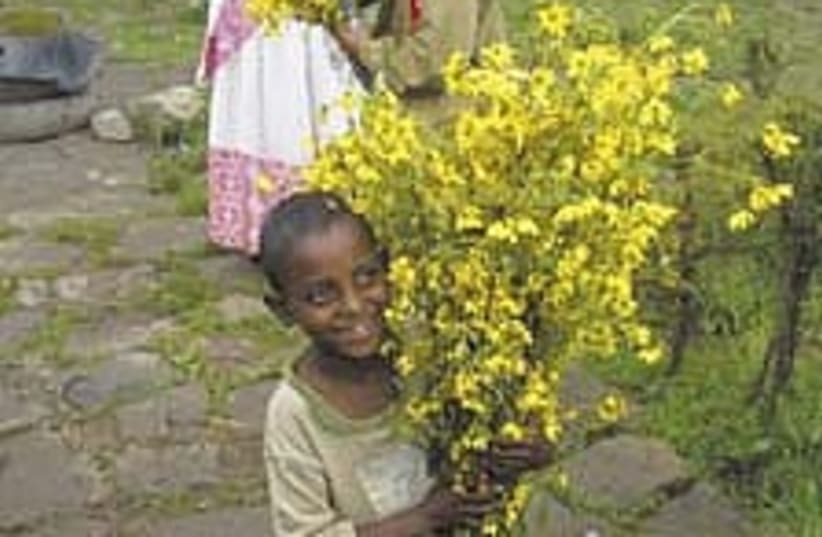
Children roamed the streets with huge bundles of the yellow Meskel flower. Meskel is an annual religious holiday celebrated by Ethiopian Orthodox Christians commemorating the "discovery of the true cross" - remnants of the cross used to crucify Jesus - by Queen Eleni during the fourth century. That evening large bonfires lit up the night sky, as people of all ages sang and danced around the fire.
Following the celebration, Tyler, Jacqueline and I met to discuss how to best make use of our time at the orphanage. Tyler has a strong background in infectious diseases and HIV. He decided to teach an HIV education class to the children that would be translated into Amharic. Jacqueline, a third-year medical student, and I set up a mini-clinic to assess any health issues. Using my digital camera, we took pictures of each child that we examined and wrote notes regarding our physical assessment.
From kwashiorkor, vitamin A deficiency, and congenital cataracts, to fungal infection, common cold and myopia, we saw a wide array of untreated illnesses and diseases - not because of neglect, but because of a lack of resources. No food and drink beyond injera (pancake-like bread from teff flour) and water. No command of the English language to understand how to use the basic medications in a donated medicine cabinet. No sewers to properly dispose human waste. No running water to take a shower or wash after using the bathroom. Access to medical care and vitamin-enriched food, elements that we consider basic for survival, were nonexistent. Moreover, there was no money to pay for any of these items that we deem necessities in our own lives.
During my final minutes at the orphanage, as I was leaving for Addis Ababa to spend Shabbat with Rick Hodes, a Jewish physician practicing there for more than 18 years, the unthinkable, yet not unimaginable, unfolded. I was ready to go, not only physically, but mentally too. My camping bag was fastened around my waist and shoulders and my backpack hung over my chest.
In my short period of time at the orphanage, I had felt as if I were approaching stimuli overload. Eating and dancing with 106 orphaned children and evaluating 19 children over six hours, combined with the lack of the usual amenities, had been challenging. The prospect of a home-cooked Shabbat meal, a warm shower, a clean shave and an English-speaking doctor whom I could relate to was enticing. But there would be one test to endure before I could bask in the familiar settings - one test that would alter the course of my life.
AS I TOOK one last glance under my bed and around the room, as if to bookmark the memory, I noticed that everyone was huddled in front of the makeshift office/infirmary. I sensed fear. I saw concern. And I heard anxiety.
I had not seen her before. Taller and fuller than the others, she was one of the seemingly healthy youngsters. They told me that she was about 20 years old.
The girl - whose name I never found out - was reclining in her friend's arm on a mattress. She was vomiting, breathing heavily and unable to talk. She had been stung by a bee and was in anaphylactic shock. I had seen this before. I had learned how to manage this situation. I am an EMT (emergency medical technician), I thought to myself. Without any medications, however, I was unsure where to begin. I immediately called for Hodes's advice. "This is an emergency. She needs adrenalin now. You need to get her to a pharmacy or clinic now," Hodes said to me. "Call me when you get there."
We put the girl in the back of the van that was taking me to Hodes' home and drove to the closest pharmacy. This was rural Africa. The closest pharmacy was not two minutes from the house; it was 30 grueling minutes away on a dirt path, past a security checkpoint and we were moving no more than 45 kilometers per hour.
In the back of the van, I took vitals every two minutes. No stethoscope, no blood pressure cuff, no oxygen. We bounced up, down and sideways. We looked in each other's eyes. I rubbed her arm, hoping that she would understand my best attempts to soothe her. She mumbled something in Amharic and her friend translated, "The bee sting me, but I will beat it."
Her respirations were rapidly rising, from 60 to 90 per minute over a 20-minute period. She was sweating through her blue shirt. The sweat was beading down her neck. Her eyes were half shut, as if she had started to move in and out of consciousness.
I'm going to have to do CPR, I recall saying to myself. How would I do CPR? Of course, I know how, but would I put my mouth over her mouth? We're in Africa. I don't know what diseases she may have. But, if I don't, she may die. These thoughts sped through my head during our grueling ride.
On the way to the pharmacy, Hodes and I mapped out a plan. Thankfully, the pharmacist spoke fluent English. I injected the first dose of epinephrine intramuscularly into the mid-lateral portion of her thigh. No response.
"Can you give it intravenously?" Hodes asked.
"Well, I can find a vein. I was trained in phlebotomy for a research project," I responded, perhaps hesitantly.
"Okay, you don't have..." Hodes started.
"No, I can do it," I replied.
I quickly took off my shirt and tied it around her arm to make a tourniquet. Her vein popped out. Beautiful, I thought to myself. Beautiful may sound like an inappropriate word at this moment, however when you learn to draw blood from sick patients, whose veins have been stabbed hundreds of times and no matter how hard you pull the tourniquet the vein is still elusive, it can be quite frustrating. Hence, it is, indeed, beautiful when a vein pops out so easily, especially when time is of the essence.
After I injected the epinephrine and corticosteroids, she began to stabilize. We bought additional epinephrine, two liters of normal saline for an IV and brought her to a local clinic. The nurse hooked her up to the IV, as the girl's fortunes began to reverse.
With Rick's approval, I continued forward for the home-cooked Shabbat meal. I appreciated it more than ever.
if(catID != 151){
var cont = `Take Israel home with the new
Jerusalem Post Store
Shop now >>
`;
document.getElementById("linkPremium").innerHTML = cont;
var divWithLink = document.getElementById("premium-link");
if(divWithLink !== null && divWithLink !== 'undefined')
{
divWithLink.style.border = "solid 1px #cb0f3e";
divWithLink.style.textAlign = "center";
divWithLink.style.marginBottom = "40px";
divWithLink.style.marginTop = "40px";
divWithLink.style.width = "728px";
divWithLink.style.backgroundColor = "#3c4860";
divWithLink.style.color = "#ffffff";
}
}
(function (v, i){
});