A breakthrough achievement of converting skin samples into functional human placenta cells – creating significant implications for understanding pregnancy development, studying pregnancy-related diseases and advancing cell therapies – has been reached by researchers at the Faculty of Medicine of the Hebrew University of Jerusalem (HU).
The cell-reprogramming research, said Prof. Yossi Buganim and his team, opens new avenues for investigating the causes of infertility, complications during pregnancy and long-term health implications for both mothers and babies. The team said their findings have the potential to “revolutionize” research on placental pathologies and genetic causes and will lead to improved diagnostic tools and therapeutic interventions.
The study has just been published under the title “Pluripotency-independent induction of human trophoblast stem cells from fibroblasts” in the prestigious journal Nature Communications.
The placenta forms in the uterus during pregnancy, supplying oxygen and nutrients to the growing fetus and removing waste products from its blood. Attached to the wall of the uterus, the fetus’s umbilical cord arises from the placenta.
Cell-based therapy: Israeli researchers reach breakthrough by transforming skin cells
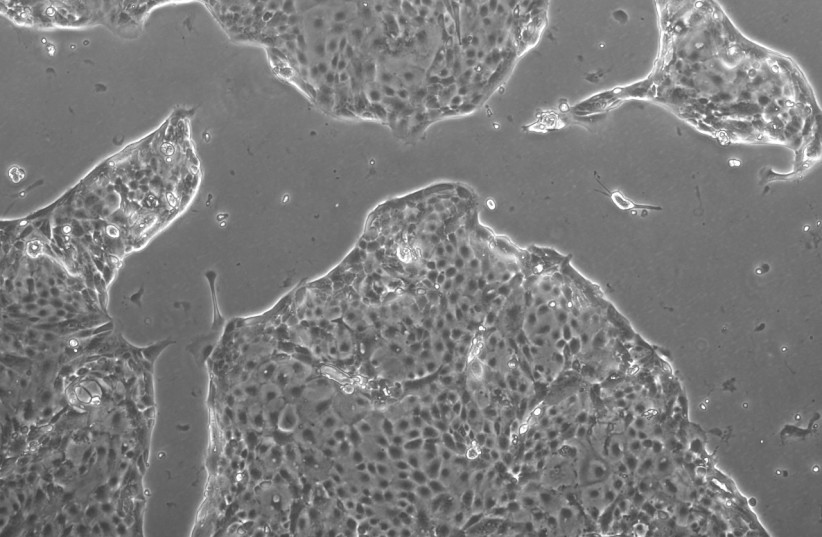
Reprogramming cells to assume new identities has been a focus of the lab that uses specialized proteins to modify gene expression. By transforming skin cells into other cell types, the team can study specific diseases and the potential development of cell-based therapies – but accessing cells from the placenta, which is a critical organ in pregnancy, has long been a challenge because of technical and ethical constraints.
The team overcame these hurdles by deriving early placental cells from skin samples to provide an unlimited supply of cells for studying the function of the placenta. Complicated pregnancies can shed light on the mechanisms behind them by using skin-derived cells with the same genetic makeup that might have contributed to placental dysfunction.
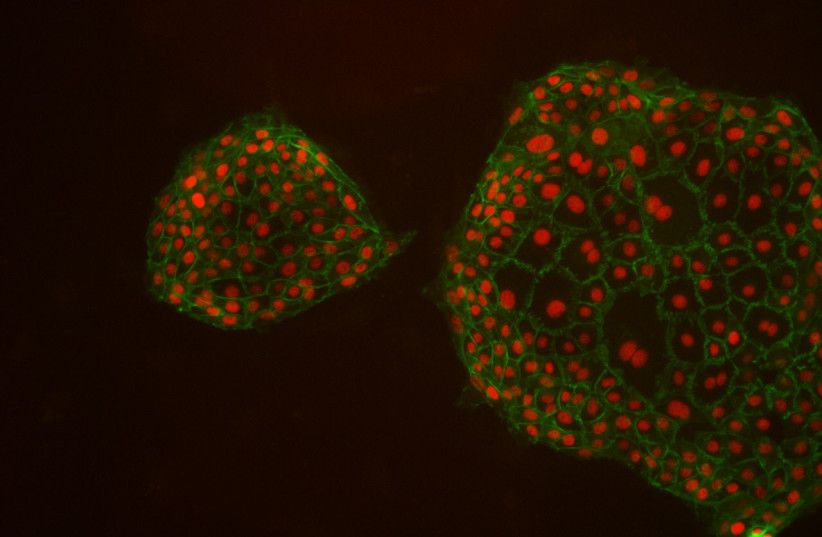
For an extensive period of time, all attempts to isolate and propagate human trophoblast stem cells (hTSCs) in vitro had failed due to a lack of knowledge of the culture conditions required for the maintenance of these cells. Recently, such culture conditions were identified and for the first time, hTSCs were successfully derived and propagated from blastocysts and first-trimester placentas.
However, this method did not allow the derivation of hTSCs from disease-affected term placentas, they wrote. “Given that placental disorders are detected only in the late stages of pregnancy, this constraint largely restricted the use of these cells in modeling placental pathologies and identifying risk factors at early stages of implantation.
Alternatively, the ability to convert fibroblasts into other cell types by a defined number of transcription factors opens an attractive avenue that resolves this limitation, as mesenchymal cells can be isolated relatively easily from post-gestational tissue, such as term placenta, cord blood or skin biopsy following disease-affected pregnancies.”
How the research team successfully converted skin cells
To achieve this, the team identified a set of genes that decide the identity of hTSCs, the precursor cells responsible for placental development. By inducing the expression of these genes in skin cells, the researchers successfully converted the skin cells into functional and stable placental stem cells. These induced placental stem cells showed similar properties to those in cells obtained from early pregnancies and had the ability to give rise to different placental cell subtypes.
Comprehensive analyses, including multi-omics comparisons (multiple omics provide an integrated perspective to power discovery across multiple levels of biology) validated the superiority of this method over previously published approaches.
The project was led by Dr. Moriyah Naama, an MD/Ph.D. program participant at HU, in collaboration with Moran Rahamim, a doctoral student, and other members of the Buganim lab. The scientists utilized over-the-counter pregnancy tests to evaluate quickly their reprogrammed cells, as these cells produce various pregnancy hormones including human chorionic gonadotropin (hCG).
The team received important guidance from Prof. Simcha Yagel’s lab at the Hadassah Medical Organization’s obstetrics and gynecology department and the Stem Cell Research Laboratory at Shaare Zedek Medical Center (SZMC) led by Prof. Rachel Eiges that provided valuable insights and provided critical samples from PGD-embryos.
