Congenital central hypoventilation syndrome (CCHS) – also known as “Ondine’s curse” after a German myth in which Ondine curses her unfaithful husband to stop breathing if he falls asleep – is a very rare neurological disorder characterized by inadequate breathing during sleep and in more severely affected individuals, during waking periods as well.
It affects about one in 148,000 to 200,000 live births and some 1,300 people living around the world. The lifelong condition is unpleasant, but with proper treatment, it does not alter life expectancy. More than 90% of cases result from new mutations in the PHOX2B gene in people with no history of the disorder in their family. Occasionally an affected person inherits the mutation from one affected parent.
Children with CCHS severely under-breathe when they are asleep, but breathing is not normal when they are awake either. There is no cure for CCHS, and it lasts one's entire life. There are no medicines which will correct the under-breathing problem. Therefore, these children require ventilatory assistance for life.
Both low oxygen levels and high carbon dioxide levels normally stimulate control of breathing to “kick in” and automatically cause us to breathe deeply or more often. People with severe CCHS don’t sense the need to breathe more deeply or to increase the rate of breathing when they develop hypoxemia (inadequate oxygen) or hypercarbia (an increase in carbon dioxide) in the bloodstream. For this reason, people with CCHS may be able to hold their breath for a long period of time without knowing the potential harm this can cause. Swimming therefore, is a dangerous sport for individuals with CCHS.
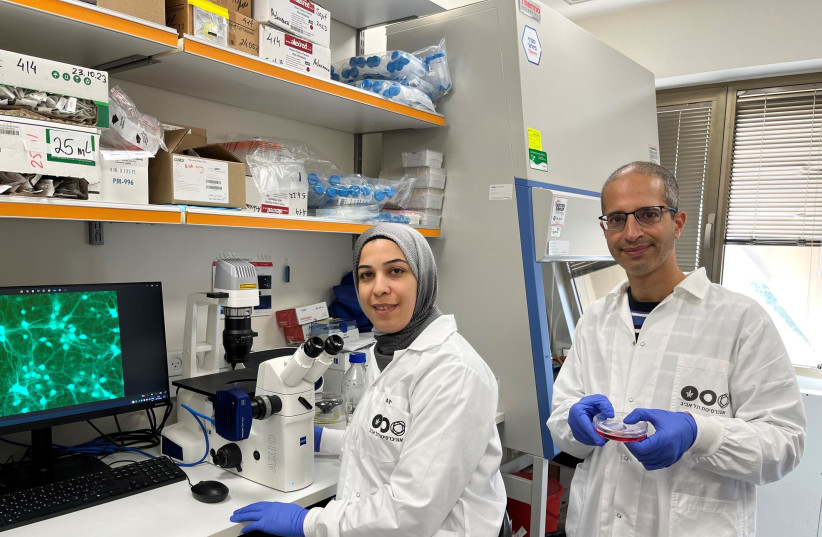
Now, Prof. Gad Vatine of Ben-Gurion University (BGU) of the Negev in Beersheba and Dr. Avraham Ashkenazi of Tel Aviv University are intensively studying the condition. Vatine is an expert in studying rare disorders using patient-specific stem cells, and Ashkenazi is an expert in tri-nucleotide repeat expansion disorders and protein clearance pathways.
Now that scientists know what's gone wrong, they can start to fix it
While they don’t work on the same diseases, the Yad Laneshima patient organization thought they could work together to find treatments for CCHS, which causes young children to stop breathing as soon as they fall asleep. This means that if they fall asleep without ventilatory support they will suffocate to death.
Sponsored initially by the Israeli organization Yad Laneshima, and then by the international CCHS Network, Vatine and Ashkenazi were intrigued by the challenge and began a collaboration. That collaboration has yielded important new information about the cause of CCHS, which could lead to future treatments.
Their findings have just been published in the prestigious EMBO journal under the title “Disease-associated polyalanine expansion mutations impair UBA6-dependent ubiquitination.”
The mutation in the PHOX2B gene is a key transcription factor in the development of the autonomic nervous system (ANS), a system that controls non-voluntary body functions such as breathing, digestion and heart rate. PHOX2B and eight other nuclear proteins that cause various neural disorders have a poly-alanine tract. In these disorders, a mutation that expands the poly-alanine tract causes the disease.
Doctoral students Fatima Amer-Sarsour from Ashkenazi’s lab at TAU and Daniel Falik from Vatine’s lab at BGU identified a poly-alanine that is also present in one of the enzymes of the ubiquitin-transfer system. Prof. Aaron Ciechanover and Prof. Avram Hershko from the Technion-Israel Institute of Technology in Haifa with the late US biologist Prof. Irwin Rose were awarded the Nobel Prize in Chemistry in 2004 for the discovery of ubiquitin-mediated protein degradation. In a healthy condition, this poly-alanine stretch is required for enzyme recognition enabling proper ubiquitin transfer to target proteins, such as those involved in neural development, thereby controlling their degradation.
In a disease like CCHS, the two research teams discovered that the expansion mutation of the poly-alanine tract in PHOX2B (and in other poly-alanine disease-causing proteins) causes aberrant interaction with the poly-alanine recognizing enzyme of the ubiquitin transfer system. This interaction disrupts the proper ubiquitin transfer to neural proteins, which inhibits the ubiquitous normal functions, leading to cell death and eventually triggering CCHS.
To make this discovery clinically relevant, the Vatine lab at the Regenerative Medicine and Stem Cell research center at BGU used patient-specific stem cells, termed induced pluripotent stem cells (iPSCs). The BGU-stem cell-core is the premier research facility of its kind in Israel, providing research support nationally and internationally. They use a technique called “reprogramming” that was developed by the Japanese Nobel Prize winner, Shinya Yamanaka. This technique enables easily accessible cells (like blood or skin cells), to be “taken back in time” to become identical to embryonic stem cells (ESCs). Unlike ESCs, iPSCs are generated without destroying embryos, and can be generated from any individual. The iPSCs from CCHS patients were then differentiated into PHOX2B-expressing cells of the ANS, which revealed the disease mechanism in the most vulnerable of the patient's nerve cells.
“Using personalized, cutting-edge technologies, we have uncovered insights that can pave the way for significant advances in the disease therapeutics,” said Falik. “I am thrilled with the progress we have made in identifying defective pathways in CCHS, as this opens up exciting research avenues to explore the development and function of the ANS,” added Amer-Sarsour.
Vatine and Ashkenazi are very excited about the potential of this groundbreaking discovery: “Now that we know what goes wrong in the CCHS patient neurons, we can start developing modalities to fix it with the goal of promoting neuron survival that will allow better quality of life for the patients,” they concluded.
