Their findings were published Friday in the prestigious peer-reviewed journal Science Advances.
This study has heavily important implications for medicine and biology.
"The field of nanotechnology took off about 20 years ago." says principal investigator Prof. Mark Schvartzman. "Nowadays, the field offers unique tools that serve scientists from many different fields. These tools allow us to create, view and control objects just 10 nanometers or less in size."
"We managed to understand how the size and physical arrangement of the receptors on the cell affect how the white blood cells 'talk to' the other cells in the body," Porgador said. "Today, cell activities within the body can be directed to fight cancer by genetically engineering receptors.
"But there is a need to develop other methods that are effective against different types of cancer," he added.
He goes on to explain that to develop other methods requires an understanding of the immune system which can be achieved through nanotechnology tools.
Lymphocytes, a type of white blood cell, are the gatekeepers of our immune system. Lymphocytes glide through the blood in the body and know how to differentiate between healthy cells and sick cells, which could turn cancerous. If the cell is identified as sick – infected by a virus or cancerous – "the patrol" breaks them up and destroys them. If the cell signals that it is healthy, the white blood cells continue as usual.
Despite the vast amount of research in the field, there are still several open questions concerning the activities of these immune checkpoint inhibitors, a breakthrough study by BGU scientists has shed light on some of these questions.
Using nanolithography, Prof. Schvartzman, a member of the Department of Materials Engineering and the Ilse Katz Institute for Nanoscale Science & Technology at BGU, developed the unique chip with metal etchings just 10 nanometers in size. The researchers then glued both types of ligands to the chip. The spacing of the ligands was varied in a controlled manner and to ensure that only one molecule attached to each receptor.
The team was able to confirm that lymphocyte cells interacted with the chip as if it were a cancerous cell and attempted to destroy it. They discovered that the distance between receptors had a dramatic effect on the lymphocytes' response: the farther away the receptors for attack and suppression, the greater the suppression. This contradicts the prevailing understanding of the scientific community, that proximity is required to suppress an attack. According to the researchers, the cell membrane has limited flexibility and therefore when the receptors are in proximity, the lymphocyte cannot attach to both receptors.
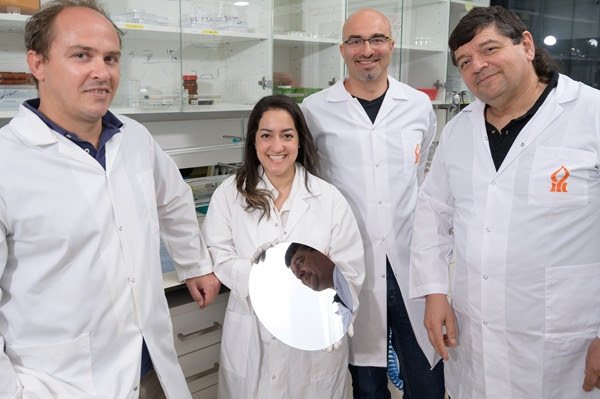
The research was carried out by doctoral student Esti Toledo and post-doc student Dr. Guillaume Le Saux with the assistance of research groups from Germany and France and was funded by the Israel Science Foundation (Grant nos. 1401/15 and 2058/18), the Ministry of Science and Technology, and the Israel Cancer Association.
