According to Prof. Eyal Mishani, the path towards opening Israel’s first “organoid” bank began as many other Hadassah Medical Center’s endeavors: a physician standing at the bedside of a patient, identifying a problem and going to the lab to find a solution.
Mishani is the Director General at the Research Fund of the Hadassah Medical Organization, and the Head of the R&D and Innovation Division.
“At Hadassah, we are very strong in translational medicine research,” Mishani said, referring to the field that sees scientific discoveries achieved in laboratories transformed into new treatments and approaches to medical care.
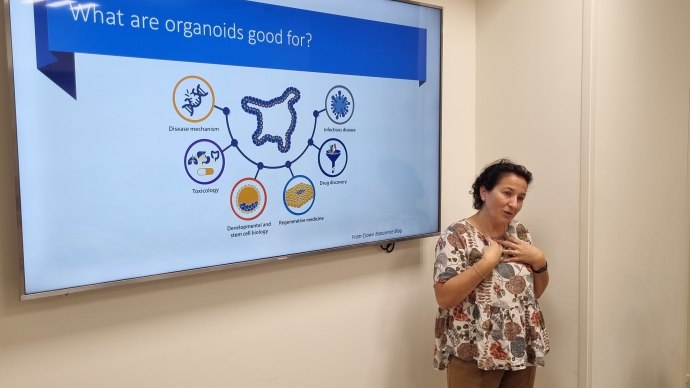
“To explain it in simple terms, organoids are lab-grown tissues that mimic the features and functions of a tissue in the body”, said Dr. Myriam Grunewald, the Director of the Organoid Center within Hadassah’s Wohl Institute for Translational Medicine.
To produce organoids, fresh biopsies are taken from different tissues in a patient’s body and then processed and grown in a special gel that allows the cells to proliferate, connect to each other and self-organize into three-dimensional structures.
Several years ago, Mishani and his team started to read scientific literature about the technology and understood its endless potential. They started to work on bringing the organoid technology that was developed by Dr. Hans Clevers and his team at the Hubrecht Institute in the Netherlands in 2009, to Hadassah.
Professor Mishani had noticed that an increasing number of laboratories around the world were working on this technology and he believed that Hadassah could take its potential to the next level by creating a platform that would be available to the entire scientific community.
“At that point, we approached our founder and owner Hadassah - The Women's Zionist Organization of America,” he recalled. “Without their vision and support, we couldn't have made it to where we are. They backed us in every possible way, including financially and through their connections. I think that this embodies what is special about Hadassah: you come with a dream and you find the support to make it come true.”
The bio-bank was inaugurated in 2021. Since then, the team members of the Hadassah Organoid Center have been collecting samples from as many patients as possible and growing them into organoids – samples from over 135 persons so far. When possible, they sample both healthy tissue and tissue presenting the disease.
“Each organoid in the bio-bank is collected and stored through a program that also records the medical history of the individual patient,” Grunewald said. “This way, if a specific condition is being investigated, for example, colorectal cancer with specific mutations, we can use the relevant samples we have in the bank, grow the organoid and start the experiment. Since 2009, the technology has made significant progress. We are able to grow organoids from almost every tissue found in the human body.”
Hadassah’s bio-bank already serves several purposes.
Currently, the main function of the Hadassah's bio bank center is to provide a platform for general research to physicians as well as academics and pharmaceutical companies, in Israel and throughout the world.
“I believe our bio-bank will become an essential tool for the industry, especially as we develop it and increase the number of samples,” said Mishani.
In addition, in specific situations, Hadassah’s physicians can already make use of the organoid center to try out treatments for specific patients and see how they will likely respond before being administered them.
“This is already happening for some cancer patients or patients with cystic fibrosis,” said Grunewald. “There is no doubt that the platform that we are developing will save precious time for patients who cannot afford the time of traditional trial and error approach.”
The hope is to expand this possibility as much as possible in the future, marking a new frontier for personalized medicine.
“Using organoids, a doctor can investigate the effect of an unlimited number of drugs on a patient, and then identify the combination of drugs that will help that individual patient,” Mishani said. “This can bring personalized medicine to a completely new level.”
For the same reason, according to the researchers, clinical trials will be dramatically impacted by organoids.
“I believe organoids will significantly reduce the need to use animals as preclinical models,” Grunewald said.
“The FDA has acknowledged the potential of organoids for drug development and testing, and has encouraged the use of these models in preclinical studies to increase the predictability and efficiency of drug development,” she added.
The dream is that the technology will go even beyond all of this.
“We can say that organoids represent the beginning of developing ex vivo organs for transplant,” said Prof. Yoram Weiss, director general of the Hadassah Medical Organization. “We are not there yet, and there is still much research to be done, but if you ask me, five or ten years down the line, there is a good chance that we will be able to transplant patient’s derived organoids to restore the function of a diseased organ. Now it might sound like science fiction, but, it is not. That future might be closer than what we think.”
This article was written in cooperation with Hadassah
