Despite the ongoing war, gynecologists and the Israel Cancer Association (ICA) are taking time to mark International Cervical Cancer Awareness Week by publicizing scientific facts and updated studies. With the help of awareness, vaccination, and early detection, cervical cancer can be eradicated in Israel, the ICA said on Monday.
In 2020, 194 countries, including Israel, resolved to eliminate a cancer for the first time and WHO launched the Global Strategy to Eliminate Cervical Cancer as a Public Health Problem.
This gynecological cancer is responsible for about 10% of new cancer cases among Israeli women. In the last decade, the number of women diagnosed here with a precancerous lesion in the cervix has increased, thanks to a rise in the performance of tests for early detection. Most of the morbidity is observed at the age of 25 to 50, and the peak of the disease being diagnosed is from the age of 30 to 34.
According to an ICA estimate, approximately 1,400 women in Israel are diagnosed with a pre-cancerous condition, and about 300 are diagnosed with invasive cervical cancer. According to Health Ministry data, in 2019, 1,381 Israeli women were diagnosed with precancerous lesions and 262 women with invasive cancer of the cervix.
ICA director-general Moshe Bar-Haim commented that “even in the shadow of the security situation, it is essential to continue the fight against cervical cancer and increase awareness of the disease. We know unequivocally that vaccination, early detection through tests and avoiding smoking dramatically reduce the risk of contracting the cancer. It can be eradicated in Israel.”
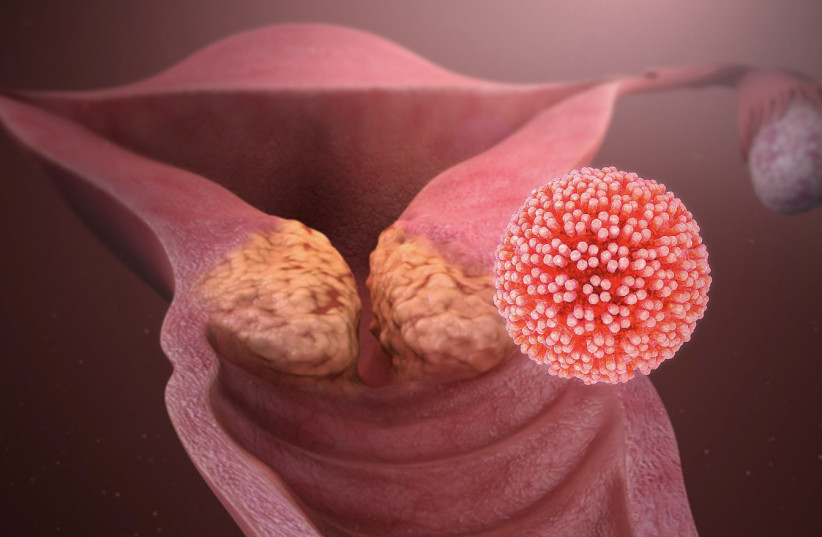
Risk factors for cervical cancer: HPV and smoking
It will be emphasized that the risk factors for cervical cancer are the human papilloma virus (HPV) and smoking. The papilloma virus damages skin cells and mucous membranes. The virus is very common in the population and is transmitted by direct contact, usually through sexual intercourse. Some strains of the virus cause warts in the genitals, while other strains are considered to have a high risk of developing pre- cancerous changes and cancer in the cervix.
Performing a cervical smear can prevent cancer. A routine examination of the cervix once every three years is the best way to detect the presence of the papilloma virus and to diagnose changes in the cervical tissue. Early detection and timely treatment will prevent the development of a cancerous tumor in this area. These periodic examinations have resulted in a significant reduction in the number of cervical cancer patients in the world.
The ICA urges women to quit smoking as an effective way to reduce the risk of cervical and other cancers and to undergo a cervical examination between ages 25 and 65. The test is included in the Basket of Health Services for women aged 25 to 54 once every three years and for women aged 55 to 65 once every five years. Women over the age of 65 who have not had an examination in the last 10 years are entitled to have one examination at no cost.
The association also urges parents to make sure to vaccinate their teenage children against the papilloma virus. The vaccine is routinely given to 8th grade students as part of the school and funded by the ministry. Those who were not vaccinated at school can receive the vaccine up to the age of 18 at ministry offices free of charge. It is important to vaccinate both girls and boys since the papilloma virus is a risk factor for morbidity not only with cervical cancer but in other types of cancer including vulvar, rectal, oral, pharyngeal, and penile cancer.
Pre-cancerous changes and early tumors of the cervix are not always accompanied by symptoms, and they are usually discovered during the recommended routine tests. The most common complaint of women with cervical cancer is irregular bleeding, such as bleeding between menstrual cycles or bleeding after intercourse. Sometimes there are also abnormal discharges from the vagina or discomfort during intercourse. There may also be bleeding among women whose menstrual cycle has stopped.
Cervical cancer shares symptoms with other conditions, but you must not ignore them
The ICA emphasizes that there are many other conditions that may cause these symptoms, but it is important not to ignore them if they appear. Therefore, every woman is urged to report them to her doctor. The earlier you meet with the doctor, the earlier the diagnosis will be made, and the chance of successful treatment will increase
The ICA offers a unique service – free sexual counseling on body image, sexuality, intimacy and fertility issues for women coping with cervical cancer, for those recovering and for patients with other types of cancer. The consultation is intended for any patient who wishes to ask questions, share the feelings of coping, receive information about the effects of the disease on sexuality and fertility, and learn about treatment options and the restoration of sexual function, as well as a referral to other professional experts. The service is provided by the association's sexuality therapist, in Hebrew, Russian and English, in a personal meeting, by phone or Zoom, free of charge and without the need for a referral. Phone: 03-5721643 or email.
A new study from Italy presents the connection between addiction to tobacco smoking and cervical cancer. From past studies, it has emerged that women who smoke are at a 70% higher risk of developing cervical cancer than women who do not smoke, but the relationship between exposure to second-hand smoke and the risk of contracting the disease has not yet been examined. In a new meta-analysis, researchers from Italy asked to check whether the risk of women who do not smoke but are exposed to secondhand smoke in their environment of getting cervical cancer and developing pre-cancerous lesions is higher than that of women who do not smoke and are not exposed to secondhand smoke.
For this purpose, the researchers examined data from 21 studies on the subject, which together included more than 5,000 cases of cervical cancer and precancerous lesions that may cause the development of cervical cancer. The data analysis showed that women who were exposed to passive smoking had a 42% higher risk of developing cervical cancer and a 50% higher risk of developing pre-cancerous lesions in the cervical region, compared to women who were not exposed.
The highest risk of getting cervical cancer exists in women who are exposed to secondhand smoke at home or to the smoking of a partner, compared to exposure at work and in the past at the parents’ home. Also, the risk of developing pre-cancerous lesions increased according to the degree of exposure to passive smoking – the number of hours of exposure to others’ smoke per day and the number of cigarettes the women were exposed to over time.
A new US study has found that the quality of the diet affects infection with the human papillomavirus. It included 10,543 women aged 18 to 59 who did not get cancer and who did not receive a vaccine against the virus. The women were tested for the presence of different strains of the papilloma virus in their bodies – strains that are defined as high risk for the development of cervical cancer and low-risk strains, as well as women without the presence of the virus strains.
Diet quality was assessed using a healthy diet index, with a higher score indicating better diet quality. According to the definitions of the index, a quality diet included several categories: vegetables, whole grains, dairy products, high-protein foods, seafood and vegetable protein, total consumption of fruit (fresh + fruit juice), fresh fruit (without fruit juice), green leafy vegetables and legumes. It was found that 25% of the women whose diet was of low quality were infected with the dangerous strains of the papilloma virus, compared to 10 % of the women who maintained a high-quality diet.
Women who consumed green leafy vegetables and legumes had a 32% lower risk of contracting the dangerous strains of the virus compared to women who did not consume these foods at all. Similarly, sufficient consumption of fruits and fruit juices compared to non-consumption reduced their risk of contracting the dangerous strains by 43%. The consumption of fruit alone also had a similar effect.
The researchers conclude that according to the study, eating enough fruits, green leafy vegetables and legumes can reduce the risk of contracting the human papilloma virus in the genitals and getting cervical cancer
