The connection between Parkinson’s disease (PD) and the extracellular matrix (ECM) in the brain has been discovered for the first time at the University of Haifa.
The ECM constitutes between 20% and 40% of the total brain volume of the developing brain in the child and adults, serving as the scaffold in which cellular components of all tissues are embedded. It’s composed of three main components – the basement membrane (basal lamina) that surrounds the cerebral vasculature; the perineuronal net that surrounds neuronal cell bodies and dendrites; and the neural interstitial matrix that is diffusely spread between the parenchymal cells.
Thanks to its varied nature and composition, the ECM can serve many functions, including the provision of support, separating the tissues from one another; and regulation of intercellular communication. The extracellular matrix therefore regulates a cell’s dynamic behavior.
A new study undertaken at the University of Haifa and just published in the prestigious journal NPJ Parkinson’s Disease under the title “Synaptic dysfunction and extracellular matrix dysregulation in dopaminergic neurons from sporadic and E326K-GBA1” has, for the first time, found a connection between PD and the ECM in the brain.
Among PD patients with a genetic background and those with sporadic PD, the researchers found evidence of changes in the genes that encode ECM proteins. “To gain a deeper understanding of Parkinson’s disease and make progress in efforts to find a cure for the disease, we need to examine the changes that occur in the extracellular matrix.
“Until now, most of the studies concerning Parkinson’s have focused on the cells and the synaptic connections. The results of our study found changes in the extracellular matrix, which have not been a focus of the Parkinson’s research,” explained study author and neurobiology Prof. Shani Stern at the Faculty of Natural Sciences’ Sagol neurobiology department.
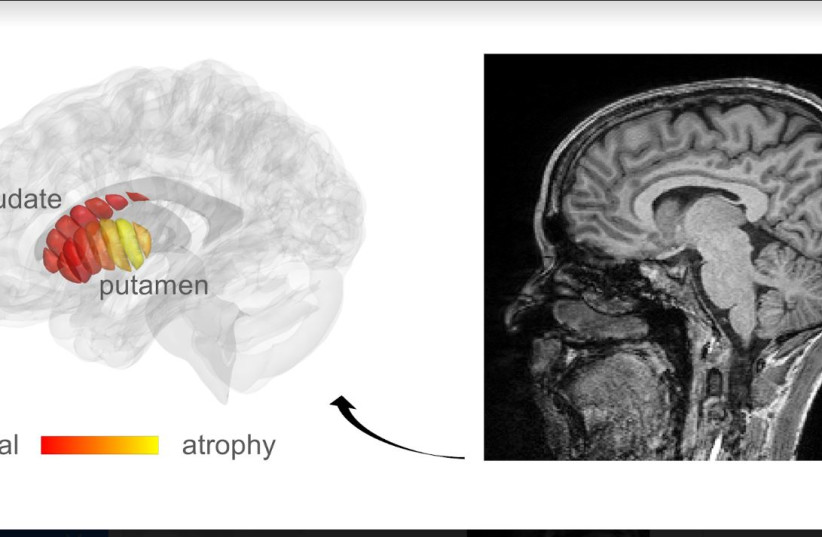
Parkinson’s disease is caused by damage to cells in the substantia nigra, an area of the brain that produces dopamine that is used to transfer reprogrammed cells into stem cells and then differentiate them as cells of a different type (dopaminergic neurons) that carry the same genetic information of the person from whom they were taken.
In this case, the researchers used samples of skin cells taken from 10 patients, some of whom are suffering from PD of genetic origin with the GBA1 gene mutation, which is associated with Gaucher’s disease. Gaucher’s patients carry a mutation in two copies of the GBA1 gene; if a person has only one copy with a mutation, they are at a higher risk of developing PD.
The other patients in the study had sporadic PD, with no known genetic changes or mutations. “We know that mutations in the GBA1 gene that are responsible for storage reprogrammed them into stem cells, and then differentiated them as cells of a different type (dopaminergic neurons) that carry the same genetic information of the person from whom they were taken. In this case, the researchers used samples of skin cells taken from 10 patients.
The GBA1 gene mutation is associated with Gaucher’s disease – which is the result of a buildup of fatty substances in certain organs, especially the spleen and the liver, which causes them to enlarge and whose function can be affected.
According to estimates, as many as one in three Ashkenazi Jews are carriers of the Gaucher disease. Researchers think that it and other Ashkenazi genetic diseases arise because of the common ancestry many Jews share.
Gaucher patients carry a mutation in two copies of the GBA1 gene; if a person has only one copy with the mutation, they are at an elevated risk of developing PD. “We know that mutations in the GBA1 gene are responsible for storage diseases such as Gaucher’s, and they are now also regarded as the commonest risk factor for PD,” Stern noted.
The skin cells were ‘reprogrammed’ as stem cells, which were then differentiated into dopaminergic cells so that the cells carried the same genetic information for each participant in the study. The same process was also undertaken for healthy participants who served as a control group.
Researchers have discovered additional functions of the extracellular matrix
Researchers have discovered in recent years that in addition to structural support, the extracellular matrix also fills various physiological functions and is involved in the creation and destruction of synapses (connections) among cells, the development of synapses, and synaptic plasticity. Stern added that today, the ECM is regarded as one of the four parts of the synapse: the presynaptic neuron, the postsynaptic neuron, the glial cells, and the extracellular matrix. Accordingly, the term ‘tetra-partite synapse’ is now in common use.
The findings show evidence – both among Parkinson’s patients with the GBA1 mutation and among patients with the sporadic disease – of changes in the expression of numerous genes that encode proteins of the ECM. For example, it was found that cells produced from PD patients have less mRNA and fewer proteins that build the ECM than cells produced from healthy people.
The researchers also discovered for the first time that the collagen-4 protein, which plays an important role in building the ECM, undergoes aggregation in PD patients but not in healthy individuals.
“We know that mutations in the GBA1 gene are responsible for storage diseases such as Gaucher’s, and they are now also regarded as the commonest risk factor for PD,” Stern noted.
“The changes appear at the same time in the differentiation process, when we see a decline in the synaptic activity of the neurons created from PD patients and a decline in their ability to transfer neural messages to other cells. We therefore believe there is a connection between the two processes,” she concluded.
