The growing resistance of bacteria to antibiotics worries doctors and researchers around the world. Now, an international study led by a team at Hadassah-University Medical Center and the Faculty of Dental Medicine of the Hebrew University of Jerusalem shows the potential effectiveness of PASA16 bacteriophage therapy in coping with dangerous Pseudomonas aeruginosa infections.
The study paves the way for future clinical trials and encourages further exploration of phage therapy as an alternative and auxiliary approach against antibiotic-resistant infections, the authors suggested.
Ran Nir-Paz, an associate professor of clinical microbiology and infectious diseases at Hadassah, who also works at Hebrew University and Hadassah’s Israeli Phage Therapy Center, and Dr. Ronen Hazan, from the bioresearch institute at the university’s dental school, headed the team that published the study in the journal Clinical Advances. It was entitled “Refractory Pseudomonas aeruginosa infections treated with phage PASA16: A compassionate-use case series.”
How can viruses be used to help where antibiotics can't?
The use of specific antibacterial viruses against infections has aroused much attention as a critical addition to conventional antibiotics, although there have been few clinical trials to test phages on patients. This was the largest study of its kind, and so far it has produced an impressive 86.6% success rate.
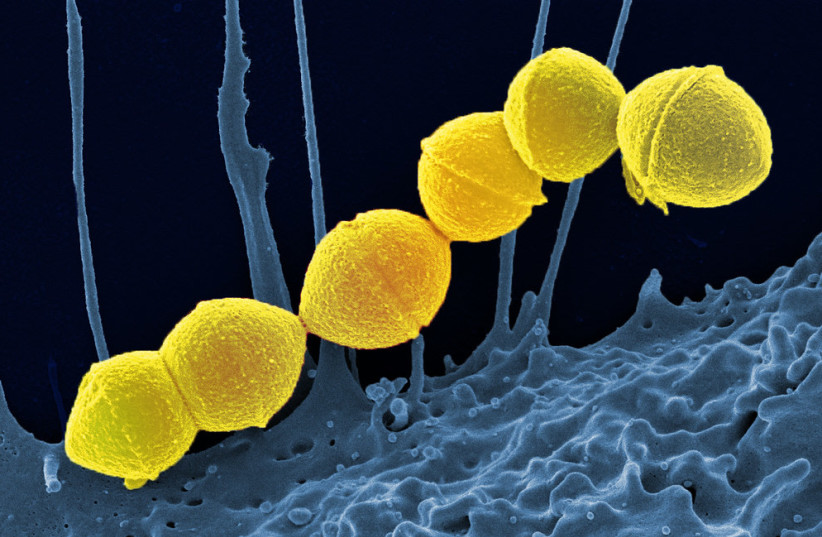
Pseudomonas aeruginosa is a bacteria found in the environment – in soil, water, and plants – and as part of bacteria in humans. It is both a pathogen and opportunistic bacteria, causing infections in patients with weakened immune systems or underlying chronic illnesses.
Before the treatment began, all Pseudomonas aeruginosa samples from patients were tested, and treatment was personalized in those who were found to be sensitive to the PASA16 phage.
During the PASA16 phage treatment, only minor and manageable side effects were observed. Remarkably, 13 out of 15 patients with available data had a favorable clinical outcome. The duration of treatment spanned from eight days to six weeks, with one- to twice-daily regimens.
This highlights the potential of combining PASA16 phage with antibiotics as a promising approach for patients with previously unsuccessful treatments.
“We are elated by the promising results of our study using phage PASA16 to treat tough Pseudomonas aeruginosa infections,” wrote the Israeli researchers, who were joined by colleagues in Israel, the US, and Australia. “This groundbreaking research offers hope for patients with persistent infections and highlights the potential of phage therapy as a valuable alternative to conventional antibiotics in combating antibiotic-resistant pathogens.”
Bacteriophage, also called phage or bacterial virus, belong to a group of viruses that infect bacteria. They were discovered independently by Frederick Twort in Great Britain in 1915 and Félix d’Hérelle in France in 1917. D’Hérelle coined the term bacteriophage, meaning “bacteria eater,” to describe the agent’s ability to destroy bacteria.
Thousands of varieties of phages exist, each of which may infect only one type or a few types of bacteria. Like all viruses, phages are simple organisms that consist of a core of genetic material (nucleic acid) surrounded by a protein capsid. The nucleic acid may be either DNA or RNA and may be double-stranded or single-stranded.
Phages have been used since the late 20th century as an alternative to antibiotics in the former Soviet Union and Central Europe, as well as in France. They are regarded as a possible therapy against multi-drug-resistant strains of many bacteria.
The authors said their work highlighted the potential of combining PASA16 phage with antibiotics as a promising approach for patients with previously unsuccessful treatments.
“By outlining potential clinical protocols, this study paves the way for future trials,” they wrote. “The success observed encourages further research and exploration of phage therapy as an alternative and complementary approach to combat antibiotic-resistant infections.”
These bacterial infections can range from mild to severe, affecting various body parts, including the lungs, urinary tract, skin, and wounds. It is a common cause of hospital-acquired infections, particularly in patients with weak immune systems or those using mechanical ventilation or invasive devices.
The pathogen’s ability to form protective biofilms hinders treatment, sometimes necessitating the combination of antibiotics and alternative therapies such as phage therapy. Strict infection-control measures in healthcare facilities are essential to combat its persistence.
The phage, which was provided pro bono by the US phage company Adaptive Phage Therapeutics, was given using various methods, including intravenous, local application to the infection site, and topical use.
