There may be only one way for humankind to survive: moving to Mars, according to Dr. Daniella Cohen, director of the Department of Community Medicine at Maccabi Health Services.
“A lot of the proponents of space exploration and habitation are based on our fear that what we are doing to our planet might actually really cause our extinction,” Cohen explained. “I think we really need to look at the stars as the future of humanity – in terms of resources, just our natural evolution, and because we are just a very curious bunch, and we need to know what is out there.”
“I think we really need to look at the stars as the future of humanity – in terms of resources, just our natural evolution, and because we are just a very curious bunch, and we need to know what is out there.”
Dr. Daniella Cohen
According to Cohen, who spoke to The Jerusalem Report on the sidelines of a two-day conference focused on “Medicine 2042,” the most optimistic prediction by Elon Musk is that there could be a human presence on Mars by 2029. Others, like NASA, believe this will happen by the mid-to-late 2030s. United Arab Emirates scientists are targeting 2117 – about 100 years from now.
“We are not talking about a mission of a few people; we are talking about having a colony. It really depends on our technological advances until then,” Cohen said. “We cannot just pitch a tent and say, ‘OK, we are here.’”
Space medicine was the topic of one of the dozens of sessions that took place in the David Intercontinental hotel in Tel Aviv from June 8-9, as part of a conference focused on the future of medicine. The event was planned shortly before the COVID-19 pandemic by Tel Aviv Sourasky Medical Center’s Nadir Arber.

Arber told the Report that even before the pandemic he grew concerned that the medical community was not planning enough for the future, so he decided to get everyone together. Hundreds of experts from Israel and around the world attended and presented at the conference.
“If you ask someone to predict what is going to happen in the coming decades, some of it will be exaggerated,” Arber said, “but against some predictions, there will be exponential advancements and we’ll accomplish much more than we could ever imagine.”
Cohen is among a select group of doctors who have been studying the challenges and opportunities of life on Mars, a planet that is located around 140 million miles away and that she described as “pretty hostile” with only 38% of Earth’s gravity and a surface temperature between 35 and -135 degrees Celsius. In addition, there is no magnetosphere, allowing levels of radiation to reach 40 to 50 times the average on Earth.
Elevated levels of radiation can cause cancer, cataracts, anxiety and burns, and can even alter human DNA.
At the same time, due to microgravity, fluid would be expected to shift away from people’s legs and travel upward toward the head, which could lead to cardiovascular changes, including reduced cardiac mass, arrhythmias, a decrease in circulating blood volume, a compensatory decrease in blood pressure and heart rate and more.
It can also lead to osteoporosis and muscle atrophy.
“As physicians, we need to think about so many aspects of health,” Cohen said. “There are acute problems, like what happens if someone has a fracture while in a space suit? But you can also be assured that if there is a colony, most definitely some of the residents will develop chronic problems such as diabetes or heart disease.”
Moreover, there are a lot of medical-ethical issues that arise around the question of fertility. People living on Mars will likely want to reproduce, but they could be bringing children into the world with genetic defects who potentially could never set foot on Earth.
“We are not sure that if they are born on Mars that their physique could adapt to the very strong gravity on Earth, they might literally break under the pressure,” Cohen added.
Finally, there are expected social and psychological issues that would arise when an exceedingly small group of people is living very far away with limited access to Earth. Presently, it takes 20 minutes each way for a message to pass between the planets, and even if modern technologies shorten that timespan, “we’re talking about a lot of isolation, a lot of self-reliance and small environments of people tend to sometimes have issues… I think depression will be one of the main things that we have to deal with.”
Could physicians help solve these challenges? Well, said Cohen, the role of the physician would have to change.
Modern medicine has grown into the realm of micro-specialization. On a Mars colony, there would likely only be a handful of doctors, so these experts would be called on to perform basic general care to potentially complex surgeries.
“We are working now on developing all kinds of virtual reality programs to help teach you very quickly how to do this or that procedure,” Cohen explained. Robotics might also come into play, where the machine is doing most of the work and the physician is the one there to aid or monitor.
However, over time, humans might adapt to this unfamiliar environment through natural or forced evolution, just as the eyes of some animals who are nocturnal adapted to the dark.
“It is speculated that Homo Martianis might be very different from us, with a much higher oxygen capacity for their lungs. They might be much shorter or squatter,” she said, adding that such a process could be hastened by mutations caused by the elevated levels of radiation, although this is only speculation.
On the other hand, perhaps new scientific techniques like CRISPR, a technology that can be used to edit genes, could enable researchers to produce embryos with huge lung capacities, strong bones and muscles, and maybe even a pigment that could protect them from radiation.
“These things are based on speculation, but that is how things start, with an idea,” Cohen said.
Just ask Dr. Eran Schenker, medical director at the Israel Aerospace Medicine Institute, who has been looking to determine the “origin of life,” as he put it, since 1996.
“Some people believe that the DNA and RNA of this society – humans and animals – arrived from other places. If this is true, it means that in other places we need to find evidence of something alive,” Schenker told the Report.
In the ‘60s and ‘70s, people spoke of aliens and UFOs. But it could be that life outside our solar system is like us or other Earth creatures.
In 2014, Japan sent a satellite to space to engage with a 1-kilometer asteroid, Schenker explained. The satellite reached the asteroid in 2019 and “kind of dived, punched the asteroid and went back.”
The satellite gathered 5 grams of small stones and placed them into a closed, secure, sterile time capsule that it then dropped back to Earth. For the past two years, researchers interested in the origins of life have been waiting for the results.
In early June they were finally revealed: There were amino acids on the asteroid.
“We did not land on an asteroid yet,” Schenker cautioned, “but maybe those amino acids really are the first signs that there are other amino acids. An amino acid is not a mineral, it is not nature, it is bio.
“I am an astrobiologist and a space doctor,” he continued. “We are looking for life outside of Earth. And this is now what we have found. It is not a definitive answer, but it is maybe [telling us] that we are not alone, which is so huge we are afraid to talk about it.”
Space tourism – the new frontier
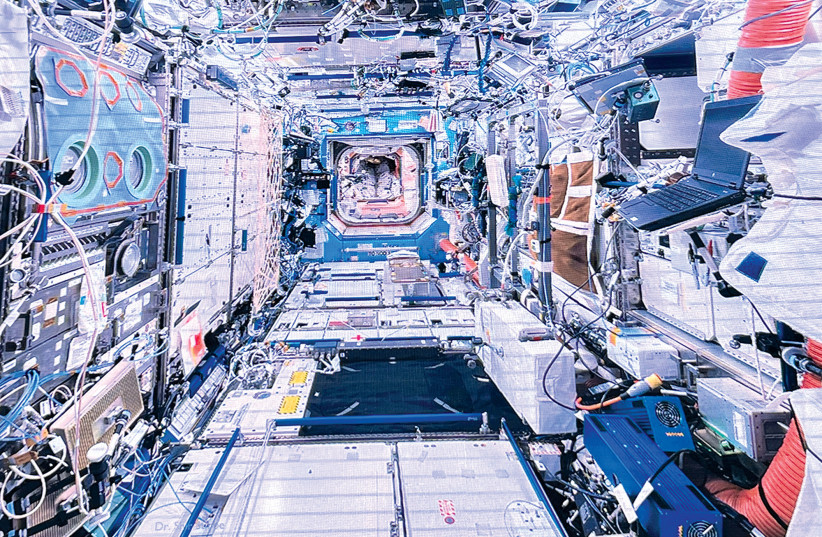
In comparison to another solar system, it would take only a few months to travel to Mars and much less time to journey to space in general. As such, before any colony is built on Mars, space tourism to the moon or space stations is likely to grow in popularity.
“Every two weeks or so, there is a space shuttle going to space with not only astronauts but people who are considered to be space tourists,” said Prof. Ran Kornowski, director of the Cardiology Center at Rabin Medical Center. He did not attend the conference but spoke separately to the Report.
Beyond his usual practice, Kornowski is practicing a more traditional form of “space medicine,” researching the impact of space on the human heart. Weightlessness in space alters the structure of the heart and the size of its chambers, he explained, and therefore candidates for space travel must undergo extensive cardiovascular testing.
Kornowski collaborated with Eytan Stibbe’s Rakia Mission and Weizmann Institute to construct a precise personal metabolic map for each astronaut; metabolic pathways mediated by the gut bacteria have been found to be connected to the cardiovascular system. The maps were compared before takeoff and on landing to help assess the change in cardiovascular risk for each astronaut.
“Most astronauts are in their 40s and have good physical status,” Kornowski said. “But over the years, we are going to have more people in their 50s, 60s or even 70s traveling to space, and the chances of them having some attack or asymptomatic cardiovascular disease is becoming more significant.”
<br>‘The next phase of innovation’
According to Sourasky Director-General Prof. Ronni Gamzu, “anything that does not look practical today, will be practical in a few years” – not just space travel. That is because, as Israel Medical Association Chair Zion Hagay explained, “medicine in 2042 will be completely revolutionary… Healthcare has entered the next phase of innovation.”
To step up care, doctors and scientists from across disciplines are converging with other specialists from engineers to mathematicians. Gamzu highlighted what he considers the “10 mega trends” of the next two decades, where advancements can be expected: digital health and artificial intelligence; omics technologies that provide the tools needed to look at the differences in DNA, RNA, proteins and other cellular molecules; molecular diagnostics and targeted treatment; nanomedicine; cell and gene therapies; stem cells and regenerative medicine; bioprinting; augmented, virtual, real view and molecular imaging; robotics; and sensors and monitors.
These advancements will improve healthcare and patient outcomes, Gamzu said.
Greece’s Prof. Sotirios Tsiodras, the chief scientific advisor for his government on COVID-19, told the Report that he believes scientists will soon be able to stop or even reverse the aging process.
Tsiodras chaired a panel on, “The new aging: Healthy 100,” that included Harvard Medical School molecular biologist David Sinclair, who recently published a report on how his team reset aging cells in mice to earlier versions of themselves using proteins that can turn an adult cell into a stem cell.
“We have the technology today to be able to go into your hundreds without worrying about getting cancer in your 70s, heart disease in your 80s and Alzheimer’s in your 90s,” Sinclair said in a video of his presentation at the 2022 Life Itself conference, shared by CNN Health.
Tsiodras said that if researchers can figure out the mechanism for cell aging, then they can prevent it – or at least help aging people enjoy healthier, higher quality, more sustainable and disease-free lives. His 2042 prediction: anti-aging vaccines.
<br>‘In need of transformation’
But there are some challenges to all of these advancements, said Dr. Jaroslaw Regula of the Institute of Oncology in Warsaw.
For starters, there could be an issue of overdiagnosis when over-screening detects diseases that would never have been symptomatic or caused death, which could lead to overtreatment. There could also be a rise in anxiety from constant monitoring, he said.
On the other hand, some people may take on more risky behaviors, feeling the implications would be caught early because they are being monitored.
Another threat with technology in medicine is cyber-attacks, which according to Arber make people more vulnerable “even than nuclear threats from Iran.”
“Let’s say the chief of staff is going to have a CT. The enemy can implant a false tumor in his head. Then, doctors will treat him, and he will die from that,” Arber described.
In general, doctors tend to be conservative and until recently were slow to pick up the use of innovative technologies and trends. However, just before the start of the pandemic in 2020, it was understood that something had to change, according to Prof. Ran Balicer, Chief Innovation Officer for Clalit Health Services.
“Demand was going up, as the population was growing and people were living longer,” he said. “Technology costs were exceedingly costly and difficult to introduce into a system that was already burdened. Patient expectations continued to mount and all the while, the amount of healthcare staff per patient was continuously declining.”
The healthcare world could not simply “go digital,” he explained. “It was in need of transformation.”
In Israel, Clalit helped lead this paradigm shift, moving from patient-level reactive therapeutics to population health – being predictive, proactive and preventative, Balicer said. To do so, the fund harnessed the power of artificial intelligence and in 2015 introduced its first predictive model for flu, whereby the fund would call patients and encourage them to get flu vaccines based not on a random system or solely on age, but on their expected risk for developing winter morbidity.
Later, it rolled out similar strategies for patients at risk of developing diabetes, stroke or other diseases.
“This is where the future lies,” Balicer said.
<br>From ‘quit or die’ to harm reduction
There will also be a focus on harm reduction – working with patients without judgment.
“We have to accept that people do things that harm them,” London oncologist Dr. Peter Harper told the Report. “We accept that people drive fast, so we put seat belts and airbags in cars. We also have to accept that people smoke and should look for less harmful alternatives [rather than a] quit or die mentality.”
He said that in 1990, the most common cause of cancer death was lung cancer, of which 80% is caused by smoking, and the same is true today.“The strategies that we have tried to implement to help people quit smoking have failed,” he said, adding that 64% of patients with lung cancer will continue to smoke until their death.
As such, “we need to give people what they want with less or no carcinogens.” In the case of cigarettes, the carcinogen is smoke.
Today, there are several alternatives, and Harper and his colleagues – French oncologist Dr. David Khayat and Moroccan urologist Prof. Redouane Rabii – said these and newer alternatives should be studied and promoted.
One alternative is electronic cigarettes, which according to the Centers for Disease Control and Prevention still have cancer-causing chemicals and tiny particles that reach deep into the lungs, but fewer than smoke from burned tobacco products.
Another is known as “heat-not-burn” tobacco products, electronic devices that have tobacco but heat it to a high temperature without setting it alight and creating the smoke that users suck in. New research is starting to show that these products are “slightly less” harmful to one’s health than cigarettes, Khayat said.
A final offering is Snus, an oral smokeless tobacco product that is usually placed behind the upper lip. It is popular in Sweden, the country with the lowest tobacco-related deaths anywhere in the world, the researchers said.
In Japan, which has recently put a focus on cigarette alternatives, a new study has shown that cardiac admissions dropped in direct relation, Harper added.
Rabii, the only Moroccan at the event, is now engaged in a study to see if these alternatives also reduce bladder cancer. He told the Report that his team will be collaborating with Israel among other countries on the study.
“If we accept innovation in heart disease, why should we not accept technical innovation in the field of tobacco smoking?” Khayat asked.
<br>Face transplantation
Another area of innovation is in the realms of autotransplantation – transplanting tissue from one part of the body to another in the same individual – and allotransplantation – transplanting tissue or an organ from one individual to another.
“Individuals can be born with a devastating malformation or go through an experience that causes a devastating distortion,” said Prof. Eyal Gur, director of the Department of Reconstructive and Aesthetic Surgery at Sourasky. “The question is can we operate and bring those individuals back to normality?”
He spoke about advances in reconstructive microsurgery, the art of putting together exceedingly small blood vessels and nerves – smaller than 1 millimeter in size – and the ability to transfer body parts from a place where they are needed less to a place where they are needed more without injuring the organ or the area from which it was taken. When done properly, the individual can regain functionality and sometimes even aesthetics, Gur said.
He shared an example of advanced microsurgery construction for facial paralysis – patients who have lost their ability to smile or use their face on one side. In this case, a sensory nerve from the foot and a mini muscle from the thigh, as well as some veins, are transferred to a healthy nerve moved from the healthy side of the face to the other.
“When it’s all done, the smile on the healthy side will create a smile or motion on the affected side,” he said.
And what if one could transplant a whole face?
So far, 46 faces have been transplanted worldwide, according to Gur. Most of these operations are called composite transplants and involve transplanting not only the skin but also underlying soft tissues.
The challenge here is that there are not enough faces. When there is one available, doctors have less than a day to find a match, and those who did receive a face transplant need life-long immunosuppression in order to keep the organ in place. Rejection is a major phenomenon in around 85% of all patients. But the drugs used as immunosuppressants are carcinogenic and often come with severe side effects.
In addition, there is mounting evidence of the extremely fast aging of those faces and ethical and aesthetic challenges. The donors need to be reconstructed enough that they can be buried looking dignified. The patients won’t look like themselves, but they also cannot look like the person who donated the face.
“We are working on models of re-educating recipients’ immune systems with novel therapies,” Gur shared.
Moreover, his team is focused on what is known as cryopreservation, a method of deep freezing and then gradually thawing organs that could give doctors more time to find a match or, in the case of a terror attack, allow a person’s limb to be frozen until he is out of danger from other injuries and able to accept the transplant.
Until now, cryopreserving has mostly been done for eggs to aid in female reproduction. The question is if it can work for larger organs. If so, then limbs would be stored in organ banks.
Gur shared a recent rodent study in which a mouse’s leg was removed, cryopreserved, and then underwent a two-stage gradual thawing process before being re-attached. It worked.
In the future, he plans large animal studies and eventually clinical human trials.
Arber said that a number of action items resulted from the conference.
“We have to get ready,” he concluded. ■
