Just as we began to believe that the shadow of the COVID-19 pandemic had lifted, the world finds itself once more in the throes of a viral resurgence.
This time, however, scientists are better positioned to use the opportunity to understand why the virus persistently mutates, with the optimistic goal of eventually thwarting its evolution.
The progress of modern medicine and technology has afforded individuals, including those with severe diseases, the opportunity to live longer – showcasing remarkable achievements within the medical and scientific communities while also presenting them with complex challenges.
One of the latest revelations in the ongoing battle against COVID-19 underscores this disquieting phenomenon.
The cycle of contagion: COVID mutations fester in immunocompromised hosts
These waves of infection, including the recent surge of the BA.2.86 variant, often originate in individuals with compromised immune systems who unwittingly serve as reservoirs for the virus, allowing it to persist and mutate within their bodies over an extended period. This protracted viral presence within them sets the stage for unwitting transmission to their family, friends, and colleagues, perpetuating the cycle of contagion.
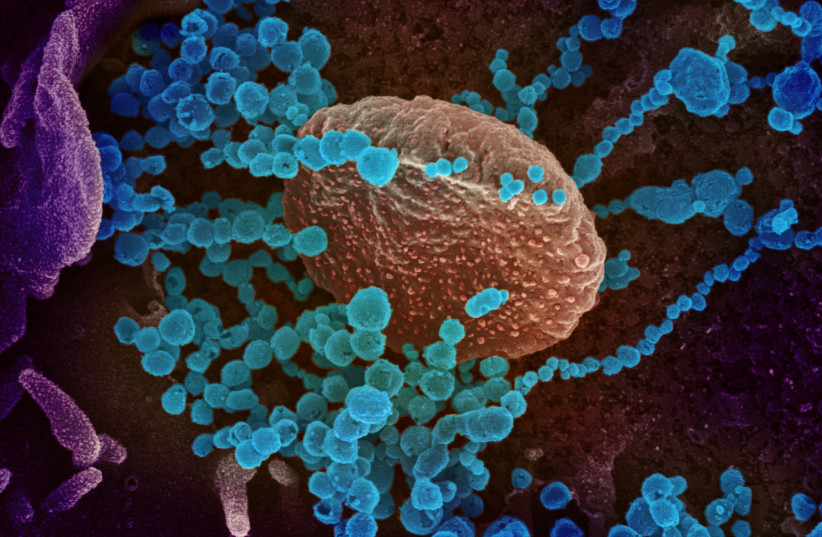
Thirty years ago, people with cancer would die after a few months. Today, such people survive. But they live with immunocompromised systems and are therefore vulnerable to viral and bacterial attack, says Dr. Nadav Sorek, the manager of the clinical microbiology laboratory and the lab for infectious disease outbreaks at Assuta Ashdod Hospital. In the case of COVID, when these people become infected, they carry the disease for longer, during which time the virus mutates, meaning it changes in their bodies.
“If you are a healthy person who gets sick, your immune system attacks the virus, so the virus does not have time to mutate,” Sorek explains. “You may still feel sick, but within three or four days your body would have likely managed to kill the virus.
“But if you are a person whose immune system is weaker and you get infected,” he continues, “your body cannot attack the virus with the same strength. So the virus survives and accumulates mutations. That is what we are seeing with these new COVID variants.”
BA.2.86 has sent waves through the scientific community due to its extensive array of mutations. Yet, amid the apprehension it has spawned, Sorek says this variant offers a unique opportunity for researchers to unravel the mysteries behind why these mutations are occurring, potentially paving the way to curbing the relentless waves of COVID-19 – and other similar diseases.
“What the scientific world wants to investigate is if what we see with COVID was happening before, with other viruses, and we never paid attention to it,” Sorek says.
On the one hand, the latest research from the United States paints a reassuring picture.
Two teams of independent scientists assessed the efficacy of antibodies in vaccinated and previously infected individuals against various virus strains, including the heavily mutated BA.2.86, dubbed Pirola. They found that our immune systems exhibit the ability to recognize and combat this variant with impressive efficacy, mirroring, and perhaps even surpassing, their performance against the XBB variant.
Individuals who displayed the most robust immune responses to BA.2.86 were those who had experienced an infection with the XBB subvariant within the last six months.
These findings hint that the forthcoming COVID-19 vaccine updates for the fall, tailored to combat XBB.1.5, will likely offer enhanced protection against a spectrum of circulating COVID-19 lineages, including BA.2.86.
On the other hand, despite these promising findings, scientists still acknowledge that BA.2.86 is a highly mutated strain, which leaves lingering concerns that its evolving nature could bring unforeseen challenges in the future if it mutates itself into a more virulent or severe disease-causing strain.
The situation is similar to what we see with antibiotic-resistant bacteria, a challenge Sorek says should be considered on the scale of climate change.
“In 30 or 40 years, we know that humanity will face a huge problem of antibiotic resistance. We will have people with many diseases and bacterial infections, and we won’t have antibiotics to treat them,” Sorek tells the Magazine.
According to the World Health Organization, there are alarmingly high rates of resistance against antibiotics that have traditionally been the go-to treatments for common bacterial infections such as urinary tract infections, sepsis, and sexually transmitted diseases.
Research has shown that antimicrobial resistance will kill more people than cancer within the next several decades.
One of the main drivers of antimicrobial resistance is the misuse or overuse of antibiotics, which pressures bacteria to adapt to survive. Antibiotics kill some germs that cause infections, but they also kill helpful germs that protect our bodies from disease. When the antimicrobial-resistant germs survive and multiply, they have resistance traits in their DNA that can spread to other germs.
When an individual has to take antibiotics for an extended period, the bacteria – like the virus – gains more and more mutations that eventually translate into resistance.
It’s a double-edged sword: Doctors want to give their patients the best possible treatments to cure them. However, some of these treatments can have lasting and contrary effects.
The recent increase in COVID cases should not be a cause for concern for the average Israeli – at least not yet, the Health Ministry has said.
However, older people and immunocompromised people should be cautious, consider wearing masks again, and stay distant from people exhibiting symptoms of the virus, former coronavirus coordinator Prof. Salman Zarka told the Magazine last week.
Moderna and Pfizer have said their updated vaccines should be ready sometime this month. Eligible individuals at high risk for severe disease should consider another jab.
Finally, if you are sick, please stay home and make sure you are not infecting others.
The writer is deputy CEO – strategy and innovation for The Jerusalem Post and a senior correspondent. She also co-hosts the Inside Israel Innovation podcast.
