An innovative treatment for COVID-19 uses a molecular "super cork" to jam the entry point used by the SARS-CoV-2 virus to enter the cell, bypassing issues that could arise with other treatments which target a spike protein on the virus, Weizmann Institute of Science announced on Wednesday.
The treatment, described in a study published in Nature Microbiology, was developed by Weizmann researchers in collaboration with the Pasteur Institute in France and the National Institutes of Health (NIH) in the US.
Most treatments and vaccines for SARS-CoV-2 target the spike protein on the virus's outer envelope, but this protein could mutate in future variants, negatively effecting the efficacy of such treatments. The Weizmann researchers decided to take a different approach, targeting the angiotensin-converting enzyme 2 (ACE2) receptors through which the virus enters the cell. This approach is not susceptible to new variants.
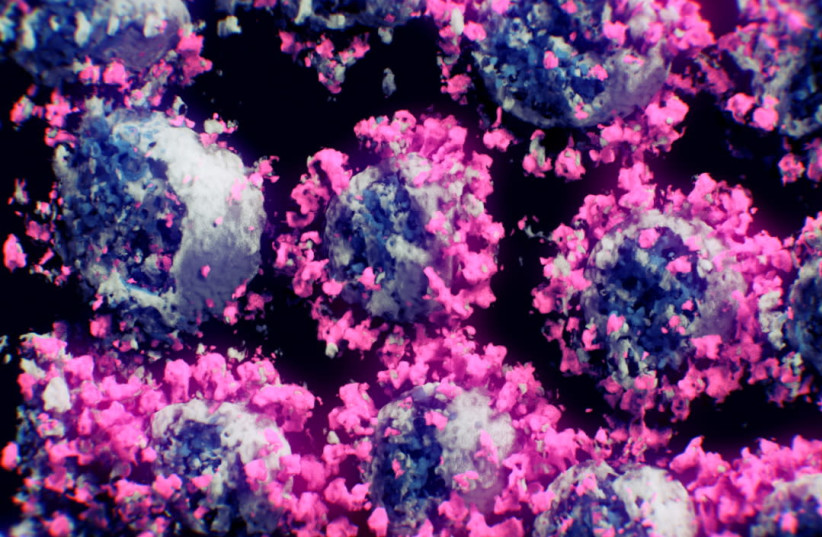
ACE2, attached to the membrane of cells on the surface of the lungs and other tissues, is an enzyme which is important for regulating blood pressure, meaning that researchers couldn't just block the receptor and disrupt ACE2's function. In order to get around this issue, the team, led by Prof. Gideon Schreiber of Weizmann’s Biomolecular Sciences Department, began developing a small protein molecule that could bind to ACE2 better than the coronavirus, without affecting the enzyme's function.
The researchers first identified the virus's binding domain, where the spike protein physically binds to ACE2. Dr. Jiří Zahradník, a postdoctoral fellow in Schreiber's group, then performed several rounds of "evolution-in-a-test-tube" on a genetically engineered strain of baker's yeast, which is easily manipulated. This allowed Zahradník to rapidly scan millions of different mutations that accumulated in the course of the artificial evolution.
The scanning process also supplied strong evidence in favor of the hypothesis that the novel coronavirus becomes more contagious as it mutates to have an improved fit to ACE2. After the first round of selection, the lab-made variants with tighter binding capabilities to the enzyme mimicked the mutations present in the binding domains of the most contagious SARS-CoV-2 strains circulating naturally. The Delta variant, however, relies on a different trick to be more infectious by partially evading detection by the immune system.
Zahradník eventually isolated a small protein fragment with a binding capability 1,000 times stronger than that of the original binding domain from which it evolved, fitting the ACE2 enzyme exactly while conserving its function.
Schreiber's team collaborated with Prof. Yinon Rudich of Weizmann’s Earth and Planetary Sciences Department to develop a potential method to administer the molecule as a drug, creating an aerosol-based spray that would allow the molecule to be administered by inhalation to patients.
The treatment has so far been tested on hamsters infected with the coronavirus at the NIH. Preliminary results show that the treatment significantly reduces disease symptoms, with more preclinical studies are planned to take place at the NIH in the near future.
