After two shots of the coronavirus vaccines, only a minority of renal transplant recipients – some 35% – developed neutralizing antibodies, new research conducted at the Sheba Medical has shown.
The study was carried out using the big data platform MDClone, which allowed the medical professionals to consider a very high number of parameters and identified which variables – like use of specific medications – were predictive of a weaker or stronger response.
The paper was published in the journal Transplantation, while the physicians are already working on a follow-up study considering the immune response after the booster, with possibly 86% developing antibodies.
The preliminary results are very encouraging, Dr. Tamar Hod, the lead author of the study and a nephrologist at Sheba, said.
“Renal transplants are a high-risk population for COVID-19 infection and complications, including prolonged hospitalizations and mortality,” she noted. “At the same time, these individuals don’t respond well to vaccines. With the coronavirus epidemic, therefore, it was important for us to explore the response to the vaccine.”
Patients who undergo renal transplants are prescribed immunosuppressive drugs after the surgery for the remainder of their lives, to prevent their immune system from rejecting the organ they received. This same mechanism interferes with the immune system's ability to deal with illness or to create antibodies from vaccinations.
Hod and her colleagues considered 120 patients who received a transplant.
“Thanks to MDClone, we were able to consider a very high number of clinical data and variables, date of transplant, type of donor, cause of the renal disease and more,” Hod said. “In addition, we obtained a huge amount of laboratory data, such as level of blood cells and platelets.”
According to the physician, it would not be possible to conduct a study analyzing such a high amount of information manually.
“In addition, we were able to consider the medications and dosage they were taking,” Hod remarked.
After two Pfizer shots, only 35% of the transplant recipients developed antibodies, compared to 97.5% of the individuals in the healthy control group.

In addition, the researchers were able to isolate which factors appeared to be associated with a weaker or stronger response.
“For example, we found out that those who were administered the full dosage of a specific immunosuppressive drug were less likely to develop a response, compared to those who received a reduced dosage,” Hod said.
The drug, called Mycophenolic acid, is usually given to patients in combination with two other immunosuppressive drugs to prevent their immune systems from rejecting the new organs they received.
Asked whether, based on the results, she would recommend changing the treatment of certain patients, Hod said that it is premature, and a controlled clinical study would be needed to make such a decision.
The level of hemoglobin in the blood also emerged as a variable, useful to predict a stronger or weaker response.
MDClone was established five years ago. It provides big-data solutions for healthcare systems and works with organizations in several countries, including Israel, the US and Canada.
Sheba has been working with the company for almost three years.
“All medical data from a hospital are uploaded in one database with a time stamp, which is very important,” said Dana Yaffe, a clinical researcher at MDClone. “This allows doctors to access each patient’s timeline.”
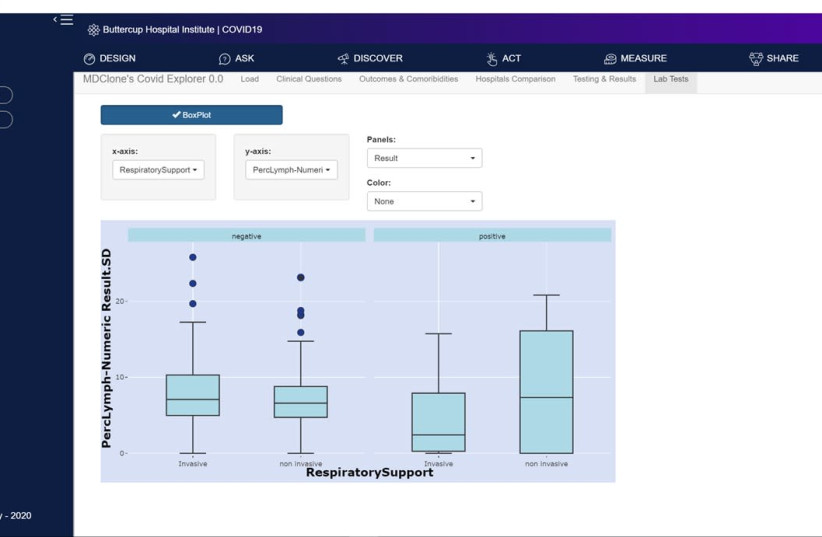
Physicians can access the data and the system autonomously. The platform receives and processes all electronic medical records, also from before the beginning of the cooperation between the company and the medical center.
Researchers at Sheba are already looking at the response of renal transplant recipients after the third vaccine, and what they are seeing has been very promising.
“The response in this case is much higher: 86% of patients developed antibodies, and those who already developed antibodies after the first two shots presented a more intense response,” Hod said. “It is a very impressive result.”
