Israeli and German scientists have identified in mice the cell of origin of combined liver/biliary duct carcinomas – a rare type of cancer of the liver. The pro-inflammatory immune messenger interleukin 6 (IL-6) was found to be the driver of carcinogenesis, while blocking of IL-6 reduced both the number and size of tumors in mice.
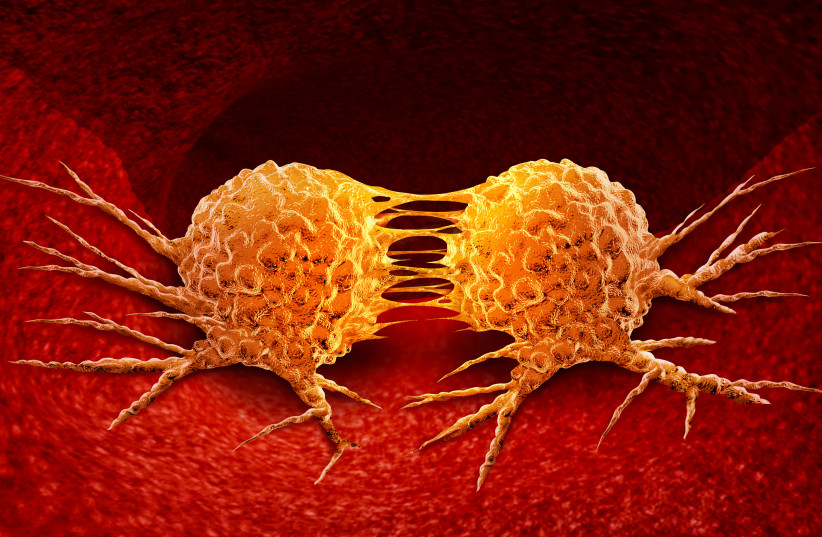
The term “liver cancer” includes hepatocellular carcinoma, intrahepatic carcinoma of the bile duct and a mixed form called combined liver/biliary duct carcinoma (cHCC/CCA). The cells of cHCC/CCA exhibit features of both forms of cancer. This rare cHCC/CCA is considered very aggressive and responds extremely poorly to current treatments.
Genes in which acquired mutations are causally linked to cancer progression are known as drivers. Cancer driver genes can be functionally classified as tumor suppressor genes or oncogenes based on their role in disease formation.
What was their study?
Scientists from the Hebrew University of Jerusalem and the German Cancer Research Center (Deutsches Krebsforschungszentrum, DKFZ) searched for the cellular origin of these tumors and sought to identify potential targets for new therapies. They published their findings in the Journal of Hepatology under the title “Combined hepatocellular-cholangiocarcinoma derives from liver progenitor cells and depends on senescence and IL6 trans-signaling.”
A team led by Prof. Eithan Galun of Hebrew University and Prof. Mathias Heikenwälder of the DKFZ conducted their studies in mice that were genetically modified to develop chronic liver inflammation and hepatocellular carcinoma at an older age, and later also developed cHCC/CCA. The molecular profile of the cHCC/CCA tumor cells in these animals largely matched that of human cHCC/CCA cells.
The joint team found that cHCC/CCA develops from degenerate liver cell precursors. In contrast, hepatocellular carcinoma most likely arises from damaged mature liver cells.
They found that in cHCC/CCA cells, genes of the pro-inflammatory interleukin 6 (IL-6) signaling pathway are particularly active. The source of the IL-6 that activates this signaling pathway are aging immune cells. The hallmark of cell aging, which scientists refer to as “senescence,” is the release of a whole cocktail of pro-inflammatory signaling molecules, among which IL-6 plays the main role.

Blocking of IL-6 action by specific antibodies reduced both the number and size of cHCC/CCA tumors in the mice. An agent that drives senescent cells into programmed cell death (apoptosis), thereby drying up the source of IL-6, also inhibited the development of cHCC/CCA.
Today, the most effective therapy for cHCC/CCA is the surgical removal of the tumors, but it is successful only if the cancer is detected at a very early stage.
“Blocking of IL-6 or agents that kill senescent IL-6-producing cells could now be further tested as promising treatment approaches against this type of cancer,” the researchers wrote. “There is now growing evidence that tumors actually diagnosed as hepatocellular carcinoma also partially contain cells of a cHCC/CCA. This means that potential therapeutic approaches against cHCC/CCA could also benefit some patients with hepatocellular cancer.”
